How to Design Emergency, ICU, OT & OPD Layouts (2026 Guide)
Table of content
Designing a hospital is not just about placing rooms on a floor plan — it’s about engineering patient safety, clinical efficiency, and zero-error workflows. And nowhere is this more important than in the Emergency, ICU, OT and OPD layouts. These four departments define how quickly a patient is diagnosed, treated, stabilised and discharged, which is why modern hospital layout design focuses heavily on patient flow, zoning, infection control and clean–dirty segregation.
Whether you are planning a new facility or upgrading an existing one, getting the ICU layout, emergency department design, OT complex layout, and OPD layout design right from Day 1 saves enormous time, cost and rework. In India, hospital promoters and architects rely on guidelines such as NABH, NBC Part 4, HFG-India and WHO emergency-care frameworks to define bed spacing, circulation routes, triage zones, scrub areas, pressure differentials and staff workflows.
This guide breaks down exactly how to design these four critical departments using practical, real-world planning principles and India-specific norms — so that your hospital is safe, future-ready and operationally efficient from the very first patient.
Getting Delays? See how to estimate construction timelines
Across Emergency, ICU, OT and OPD layouts, four universal principles of good hospital layout design always apply. These principles directly influence patient flow, infection control, and overall clinical efficiency.
1. Separate All Circulation Flows Clearly
Every hospital must separate:
- Public/patient movement
- Staff movement
- Clean supply routes
- Dirty/soiled & biomedical waste routes
Clear segregation reduces infection risk, prevents cross-movement, and makes NABH audits easier.
2. Ensure Short, Direct Connections Between Critical Departments
Life-saving departments must sit close together:
Emergency → Imaging (CT/X-ray) → OT → ICU/HDU
This reduces travel time, especially during trauma, stroke or cardiac emergencies. HFG-India also recommends direct, restricted access between emergency care areas and the OT/ICU cluster. Source
3. Use Zoning for Strong Infection Control
Every hospital layout should move from:
Public → Semi-restricted → Restricted → Sterile
This zoning is most important in:
- ICU layout design (isolation, airflow, access control)
- OT complex layout (sterile core, scrub zones, clean corridors)
Following NABH and NBC norms here is critical to reduce airborne and contact-based infections. Source
4. Consider Noise, Light & Staff Ergonomics
Clinical performance in ICUs and OTs is strongly affected by noise and lighting:
- Recommended ICU noise levels: 40–45 dBA
- Actual Indian ICUs often reach 60–90 dBA, affecting recovery and staff fatigue
Simple layout choices, placement of staff stations, corridors, doors, and equipment — significantly influence how safe, calm and efficient the environment feels.
How to get hospital license in 2026
A well-designed Emergency Department layout improves patient flow, reduces delays during the golden hour, and minimises overcrowding — a common challenge in Indian hospitals. These principles form the backbone of efficient emergency department layout design and directly impact triage accuracy, treatment speed and clinical outcomes.
1. Functional Zones Required in a Modern Emergency Unit
According to WHO and HFG-India, every Emergency Department should be divided into clearly defined zones:
2. Access, Adjacency & Flow Design
HFG-India recommends the following principles for safe emergency department layout design:
- Separate Entrances
- Ambulance entrance (restricted) and walk-in entrance (public).
Prevents stretcher congestion and improves emergency access.
- Ambulance entrance (restricted) and walk-in entrance (public).
- Controlled Access to Clinical Areas
- Public movement must not pass through triage, resuscitation or acute care bays.
- Close Adjacency to Critical Units: To reduce transfer time during trauma and cardiac emergencies, the ED should have direct or vertical access to:
- Radiology (CT, X-ray)
- Blood bank / lab
- OT complex
- ICU / HDU
- Indian Evidence: Studies show that poor ED flow in India leads to overcrowding, long triage queues and delayed imaging, significantly slowing care delivery.
- Design Tip:
- Map a patient journey from gate → triage → resus → CT → OT → ICU.
- Any unnecessary back-tracking or long travel paths indicate layout inefficiencies.
3 Area & Bed Planning Guidelines
Common planning norms (HFG-India + global references):
- Treatment Spaces
- 1 treatment space ≈ 1,000–1,500 annual ED visits.
- Resuscitation Bays: Should support
- 360° staff access
- Space for ventilator, monitor, pumps
- Work area for 4–6 clinicians at once
- Isolation-Capable Bay: Every ED should include one negative-pressure resus bay for infectious emergencies (COVID, TB, H1N1, unknown fever).
Practical Planning Note: Most Indian hospitals benefit from fewer but well-equipped resus beds rather than many under-equipped ones.
How to build a patient centric hospital in 2026
1. Space Requirements Per ICU Bed
A safe, efficient ICU layout design begins with adequate space. Most global and Indian guidelines align on the following:
2. Noise, Light & Environmental Comfort
Noise and lighting significantly impact patient recovery and staff performance:
- Recommended ICU noise: 40–45 dBA
- Actual Indian ICU noise: Often 60–90 dBA, almost double acceptable limits
Good ICU room design places noisy functions (printers, alarms, donning/doffing, supply zones) away from patient rooms.
Use:
- Sound-absorbing wall/ceiling materials
- Natural light access and external views where possible
These improve orientation, sleep cycles and reduce stress for patients and clinicians.
3. Visibility & Staff Workflow
Effective ICU layout planning must balance visibility, privacy and workflow efficiency:
- Central or decentralized nurse stations with direct sightlines to all beds (glass partitions help).
- Avoid blind spots where alarms or patient deterioration may go unnoticed.
- Each bed must have immediate access to:
- Medical gases (headwall or ceiling pendants)
- 12–20 electrical outlets
- Data/Wi-Fi ports for monitoring and HIS integration
- Medical gases (headwall or ceiling pendants)
This ensures seamless monitoring and rapid response during emergencies.
4. Infection Control & Zoning
In ICUs, infection control is a design problem as much as a clinical one:
- Separate clean and dirty utility rooms with clear signage and movement pathways.
- Handwash stations at all ICU entry points and near bed clusters (NABH requirement).
- Isolation rooms should be positioned to minimize cross-traffic, ideally at corridor ends.
- Layout should support fast donning/doffing, with PPE stations placed close to patient rooms.
Together, these measures reduce HAI risk and support compliance with NABH and international critical-care standards.
Best Hospital Construction Company for Non-Profits
The Operation Theatre (OT) complex is the most controlled, high-risk, and high-cost area of any hospital. A well-designed OT layout improves sterility, reduces infection risk, speeds up surgical turnover, and enhances safety for both patients and staff. Modern OT planning revolves around two core principles:
- Zoning
- Air and sterility control
1. The Four OT Zones (Core of OT Layout Design)
Standard OT complex design in India, as used in NABH-aligned teaching and government guidelines, divides the OT into four zones for infection control and workflow efficiency:
Adjacency requirement: The OT complex must be directly connected to CSSD, ICU/HDU, labour room, and Emergency for safe and quick patient transfer.
2. Operating Room Size & HVAC Requirements
Modern OT room design follows international & Indian HVAC standards:
- Minimum OR height: ~3 metres
- Air changes: Minimum 20 air changes per hour (ACH) in laminar-flow OTs
- Laminar airflow: Vertical airflow over the operating table to maintain a low-particulate surgical zone
- HEPA filtration: High-efficiency particulate filters with balanced exhaust and recirculation
Layout essentials inside the OR:
- Anesthesia work area + gas columns located at the head end
- Clear sterile corridor from scrub → OT entrance → surgical table
- Separated clean and dirty routes for instruments (CSSD → OT → dirty utility)
These measures reduce SSI (surgical site infection) risk and improve surgical performance.
3. Support Rooms That Determine OT Efficiency
Even the most advanced OR will underperform without the right support spaces. Efficient OT complexes include:
- Pre-op and PACU (Post-Anesthesia Care Unit) adjacent to OTs to reduce start-up and turnover time
- Instrument & linen rooms sized for peak surgical load
- Surgeon and anesthetist reporting / on-call rooms for immediate availability
- Adequate storage for sterile consumables and emergency equipment
NABH OT guidelines emphasise equipment readiness, safe storage, and unobstructed movement, which directly influences OT utilisation rates and safety.
Hospital Floor Plan Guide 2026
The OPD (Outpatient Department) shapes 70–80% of a hospital’s first impressions. Poorly planned OPDs in India often face overcrowding, long queues, and inefficient movement. A smart OPD layout design improves patient flow, reduces waiting time, and enhances overall experience.
1. OPD Load & Area Planning Norms
Standard planning guidelines for OPD layout design suggest:
2. Patient Flow & Common Bottlenecks
Studies on Indian OPDs highlight bottlenecks at:
- Registration
- Billing
- Diagnostics
These occur when all patients must pass through a single narrow corridor. Overcrowding at OPD entrances and registration counters in Indian public hospitals is widely reported, often due to inadequate waiting space and poor flow design.
Design Guidelines for Better OPD Flow//infographic
- Separate registration/billing from clinical corridors with adequate queue space
- Use single-direction patient loops:
Entry → Registration → Waiting → Consultation → Diagnostics → Pharmacy → Exit - Provide overflow waiting areas (covered outdoor verandas) for peak hours
- Use digital kiosks and online appointments, while retaining physical counters for non–tech-savvy patients
These strategies reduce congestion, improve patient satisfaction, and streamline hospital operations.
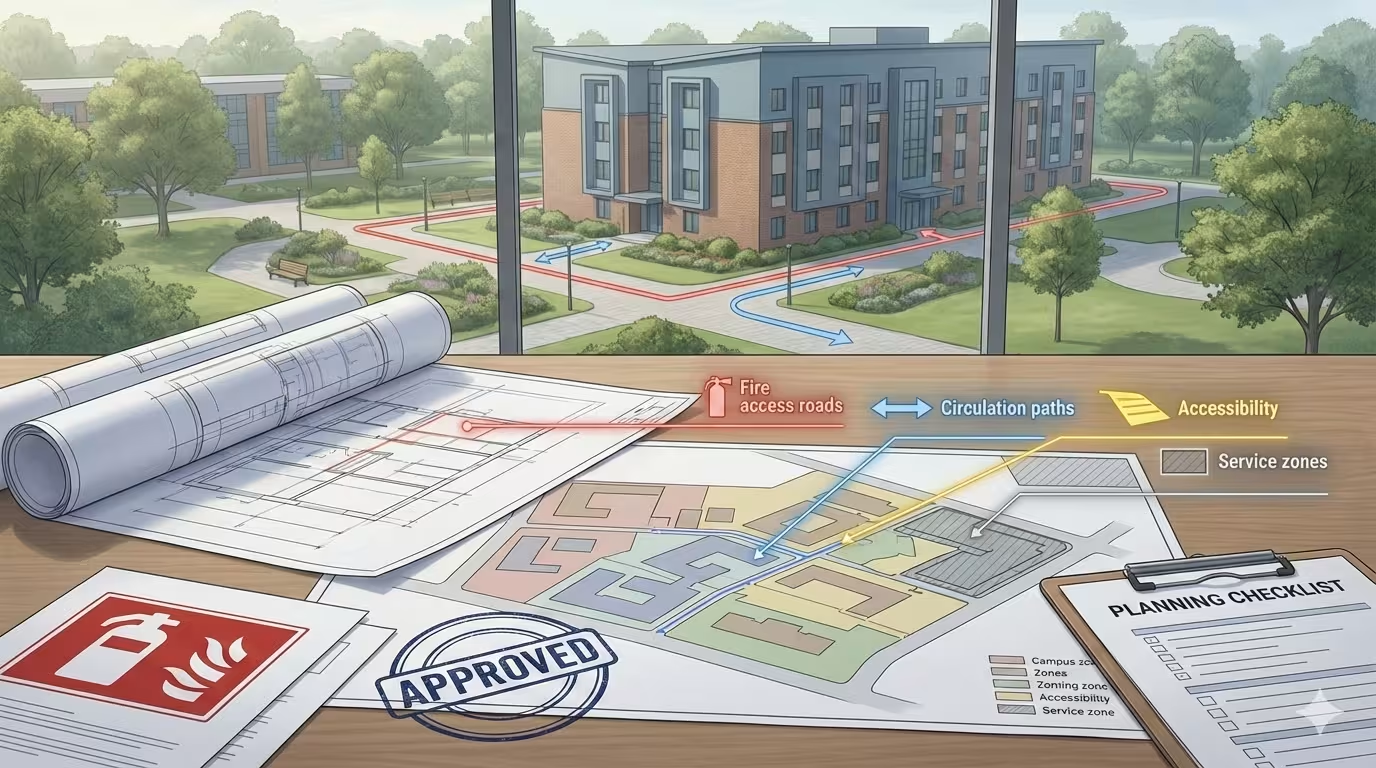
Plan a Medical College Campus in 2026
Even perfectly designed departments can fail if placed incorrectly in the hospital building. High-performing hospitals follow proven hospital master planning principles for safety, accessibility, and efficiency.(BuiltX)
- Ground / Lower Floors
- OPD, imaging, and pharmacy at ground level for easy public access
- Emergency Department layout must have a direct ambulance bay and rapid access to imaging and OTs
- Intermediate Levels
- OT complex and ICU/HDU should be vertically aligned with Emergency
- Ensure the shortest possible path from Emergency → OT → ICU for trauma, cardiac and stroke cases
- Upper Floors
- IPD wards, step-down units and long-stay beds
- Circulation Separation
- Keep public lifts and service lifts separate
- Avoid cross-traffic between clean routes and dirty / soiled routes
- Maintain clear pathways for stretcher movement and CSSD–OT connectivity
A well-structured hospital layout improves turnaround time, reduces infection risk, and enhances patient experience — making it a critical part of hospital design.
Which construction contractors will be best for your project in 2026
Infographic
A systematic process makes complex hospital layout design manageable. A typical 8-step approach:
- Functional brief workshop
- Clinicians, nursing, admin, infection control, biomedical, facility management, and fire consultants agree on bed numbers, case mix, and workflows.
- Clinicians, nursing, admin, infection control, biomedical, facility management, and fire consultants agree on bed numbers, case mix, and workflows.
- Regulatory & accreditation mapping
- Map NABH 6th Edition and relevant state fire/local building bye-laws for each of Emergency, ICU, OT, OPD.
- Map NABH 6th Edition and relevant state fire/local building bye-laws for each of Emergency, ICU, OT, OPD.
- Blocking & stacking
- Decide which departments sit where (ground / podium / tower) and how Emergency–OT–ICU connect.
- Decide which departments sit where (ground / podium / tower) and how Emergency–OT–ICU connect.
- Departmental layout options
- For each unit, create 2–3 options that respect:
- clean vs dirty flows,
- staff vs public routes,
- code-mandated exits & travel distances.
- clean vs dirty flows,
- For each unit, create 2–3 options that respect:
- Simulated patient journeys
- Use HEAT and OPD patient-flow studies as reference to test “day in the life” of trauma, ICU, surgical and OPD patients.
- Use HEAT and OPD patient-flow studies as reference to test “day in the life” of trauma, ICU, surgical and OPD patients.
- Engineering integration
- Work with MEP teams on air changes, pressure differentials for ICU/OT, emergency power to critical sockets, medical gas routing.
- Work with MEP teams on air changes, pressure differentials for ICU/OT, emergency power to critical sockets, medical gas routing.
- Mock-ups & fine-tuning
- Full-scale or 3D mock-ups of ICU bed bays, resus bays and an OR to test clearances, visibility and ergonomics against ICU and OT design guidelines.
- Full-scale or 3D mock-ups of ICU bed bays, resus bays and an OR to test clearances, visibility and ergonomics against ICU and OT design guidelines.
- Checklists & commissioning
- Use NABH ICU/OT checklists and WHO emergency tools (HEAT, triage tools) as final validation before go-live.
Top 10 Hospital Design Requirement in 2026
Designing the Emergency, ICU, OT and OPD layouts is ultimately about creating a hospital that moves patients faster, reduces infection risks, and supports clinicians at every step. When these spaces are planned with clear flows, strong zoning and the right engineering integration, hospitals simply perform better.
But turning a great hospital layout design into a high-quality, code-compliant facility needs real execution expertise. That’s where BuiltX makes the difference. With deep experience in hospital construction, OT/ICU execution and healthcare-grade MEP systems, BuiltX has become a trusted partner for organisations building modern, efficient healthcare infrastructure.
If you’re planning a new hospital or upgrading critical departments, BuiltX can help you turn your layouts into safe, future-ready spaces that work exactly as intended. Book your free call now!
Build it right. Build it future-ready. Build it with BuiltX.